In Minot, ND, population 47,800, staff at Trinity Health often face challenges when filling positions for health information (HI) professionals.
The pool of local and regional HI candidates is limited, says Deb Boppre, MSM, RHIA, CCS, CCS-P, FAHIMA, enterprise health information/clinical documentation director for Trinity Health. At the same time, the growing number of remote roles for HI professionals is frequently more appealing to job seekers than in-person roles, she says.
“People have opportunities to get better jobs all the time,” Boppre says. “Especially in a smaller community, we cannot be as competitive from a wage perspective. We’re having to compete with Minneapolis, Denver, New York, or anywhere across the country. Staffing has been a struggle.”
Similar HI staffing obstacles are playing out across the country. Of the more than 2,500 HI professionals who responded to a survey by NORC and AHIMA, two-thirds (66 percent) of respondents reported understaffing of HI professionals at their organizations within the last two years.
Boppre’s assessment of what’s driving understaffing aligns with that of survey respondents. Competitive compensation issues, limited local talent pools, challenges finding candidates with the right expertise, and preference for remote work are among the top contributors to understaffing, survey participants say.
The ever-evolving role of HI professionals also plays a part in the dilemma, says Susan W. Carey, MHIM, RHIT, FAHIMA, system vice president of IT patient services and HIM for Norton Healthcare in Louisville, KY.
“As far as we’ve come, I think HIM departments continue to morph in response to technology trends, data analytics, and regulations, and so, as we’ve said for years, there isn’t a ‘traditional HIM department,’ ” she says. “Because of this, you have varying organizational structures for HIM, and it makes it difficult to staff.”
Understaffing Often Has Detrimental Effects
From financial losses to regulatory delays to overworked teams, the impact of understaffing can run the gamut.
“One of the biggest impacts is the backlogs that you end up with because you just don’t have the staff to complete all the work that’s necessary,” Boppre says.
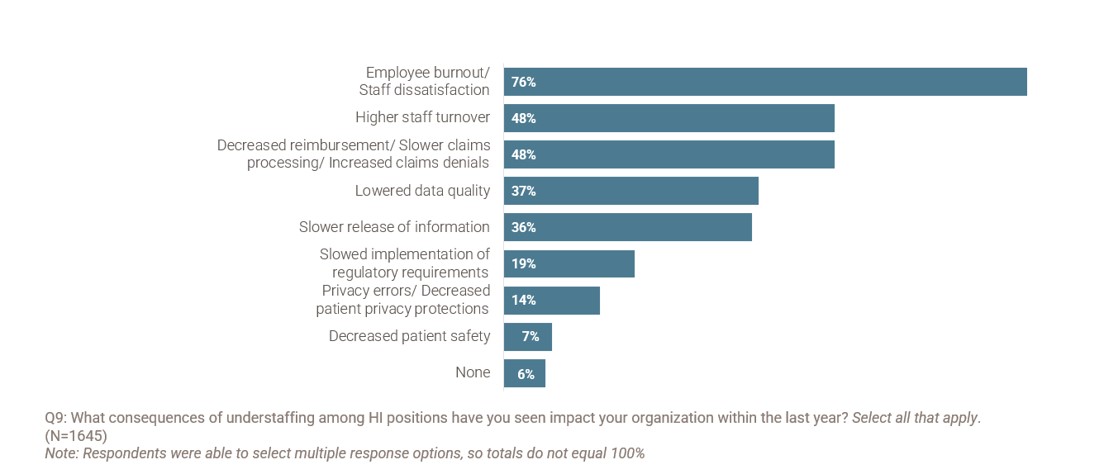
In the NORC-AHIMA workforce survey, nearly half of respondents (48 percent) reported that understaffing at their organization has led to decreased reimbursement, slower claims processing, and increased claims denials.
Source: Health Information Workforce: Survey Results on Workforce Challenges and the Role of Emerging Technologies. NORC and AHIMA. 2023
From a coding standpoint, delays caused by understaffing can have serious financial consequences, says Jami Woebkenberg, MHIM, RHIA, CPHI, FAHIMA, senior director for HIM operations at Banner Health in Phoenix, AZ.
“You need to get those accounts coded as quickly as possible and get them out the door so that you can reimbursed,” she says. “From a release of information standpoint, we need to ensure records are released in a timely manner. That can also impact reimbursement if it’s a payer or an attorney that needs to review a record before they can authorize payment.”
Slightly over one-third of survey respondents (36 percent) reported slower release of health information as an impact of understaffing at their organization. Responses indicating slower release of information were higher among organizations where 50 percent or less of HI roles required a certification.
At Boppre’s workplace, Trinity Health, leaders have resorted to outsource support for some coding functions. Other functions, such as document imaging and release of information, are done internally, and in some cases, managers must pay staff overtime to get the work done.
“That’s more cost to our organization,” she says. “It’s not a permanent solution to a challenging, ongoing problem.”
Mental exhaustion and low morale are two other consequences of understaffing. Among survey respondents, 76 percent identified “employee burnout” and “staff dissatisfaction” as results of understaffing. Higher staff turnover was a common result of understaffing, according to respondents.
“You spend a lot of money training and getting staff up to speed, then that talent walks out the door. It’s tough to deal with,” Carey says. “Turnover is costly because you need to have staff come in and supplement while you recruit. You may have to bring in temp staffing depending on how quickly you can staff your positions.”
Lack of staff can also impede efficiency and advancement, adds Sandy Pearson, MHA, RHIA, CHDA, vice president of enterprise health information management at Intermountain Health in Broomfield, CO.
“We spend so much time covering gaps that we don’t have time to streamline, optimize, or automate,” she says.
The completeness and timeliness of electronic health record (EHR) data can also be affected, Woebkenberg notes.
“Physicians need those records in order to treat patients,” she says. “Ensuring that we’ve got information in the EHR available for patient care, whether it’s physicians or other clinicians, that piece is important as well.”
In addition, privacy errors and decreasedpatient privacy protections result from understaffing, according to survey respondents. Seven percent of respondents also reported decreased patient safety was an impact of understaffing at their organization.
Improving Staffing Through Communication, Flexibility
To address staffing challenges, Woebkenberg and Carey recommend working regularly with human resources and recruiters to ensure job descriptions are up to date, minimum qualifications are clear, and top candidates are a good fit.
“The other [element] is helping our leadership, who is responsible for approving replacement and new positions, understand the impact HIM staff have on the organization,” Woebkenberg says.
Sometimes, misconceptions exist among some leadership as to the value of non-clinical roles such as HI and how they affect healthcare within an organization, she says. It’s critical that leaders recognize the impact health information has on patient care, patient safety, and financial outcomes, adds Woebkenberg.
Pearson suggests that teams look toward automation to make staffing go farther and allow for more remote work, when possible. Pearson’s team, for example, is considering implementing a system that automatically moves some items out of work queues using specific criteria, removing the need for manual touching.
Despite the staffing challenges her team faces, Boppre says her department’s turnover rate is less than three percent. She attributes the success to her strong leadership team and their focus on staff communication.
“One of the things that helps us continue to maintain our team is our communication and our openness,” she says. “We are upfront with our staff and [share] any struggles we’re going through. It helps them feel more connected.”
Working with schools and helping train students for HI positions also offers solutions. For example, Norton Healthcare partners with a local university for an annual program that provides tuition assistance to students who want to obtain their registered health information technician (RHIT) certification.
“This helps with their career path and also helps staffing because when you have higher level positions open, you’ve got folks to move into them right away,” Carey says.
To address understaffing, the NORC-AHIMA workforce report recommends that Congress allocate a portion of new and existing grants within the US Department of Health and Human Services (HHS) for HI education, training, and certification programs. Specifically, grants should be provided through the Health Resources and Services Administration (HRSA) to support training and education for HI professionals, especially those in rural and underserved areas, according to the report.
In addition, HHS could collaborate with the US Department of Education to fund scholarships for undergraduate and graduate programs and, in collaboration with the US Department of Labor, develop apprenticeship opportunities for individuals interested in pursuing a career in health information, the report advises.
Keeping pay and benefits for HI professionals competitive is also essential, Pearson adds.
“Every employee’s priority for their position is different,” she says. “For some it’s pay, for others its opportunity and advancement. For some, it’s recognition and wanting to do a good job. There are countless things that motivate and retain people. Finding a balance and targeting each individual’s motivator, if you can, is key.”
Alicia Gallegos is a freelance healthcare journalist based in the Midwest.
Take the CE Quiz