
UCLA's Journey to Using SDOH Data to Improve Outcomes and Health Equity
Join Dr. Medell Briggs-Malonson, chief of health equity, diversity, and inclusion for the UCLA Health System and AHIMA President/Chair-elect Maria Caban Alizondo for a lively conversation about UCLA Health System's journey to use social determinants of health (SDOH) data they have gathered from their patients and community to improve health and healthcare outcomes. The free, live webinar is on Feb. 16 at 12 p.m. CT.
Sign up today
Like many health systems nationwide, Livonia, Michigan-based Trinity Health recognized the importance of social needs data, yet it faced many challenges collecting it — particularly getting patient buy-in. Trinity Health operates 89 hospitals and care centers in 22 states.
Cristina Spurlin, senior program consultant for health equity and population health, and Zakiya Suleiman, senior program consultant of social care data, and technology, share insights into Trinity Health’s journey thus far.
Q: How does Trinity Health collect SDOH data?
Suleiman: Trinity Health uses the term social influencers of health (SIOH) rather than determinants because while community conditions can influence a person’s ability to be healthy, there are opportunities to shift rather than determine a person’s health. Trinity Health actively screens and addresses patient social needs through multisector collaborations in the communities we serve.
Trinity Health created a standardized patient social needs screening tool that’s available in 15 languages. We use it primarily in the ambulatory setting and are rolling it out broadly in inpatient settings.
Q: How did you develop the tool?
Suleiman: We formed a multi-disciplinary team lead by our Community Health and Well-Being department that includes health information, health informatics, and clinical colleagues. This team reviewed nationally validated screening questions, as well as Epic electronic health record (EHR) foundation social needs questions, to create our own unique set of questions.
We found that validated questions don’t necessarily take health literacy into consideration. Using a health and racial equity lens, the tool is deployed differently depending on the patient and their reading literacy and health literacy. Patients can complete the assessment on their own, or our medical assistants, community health workers, social workers, and care managers ask the questions and then input information into discrete fields in the EHR.
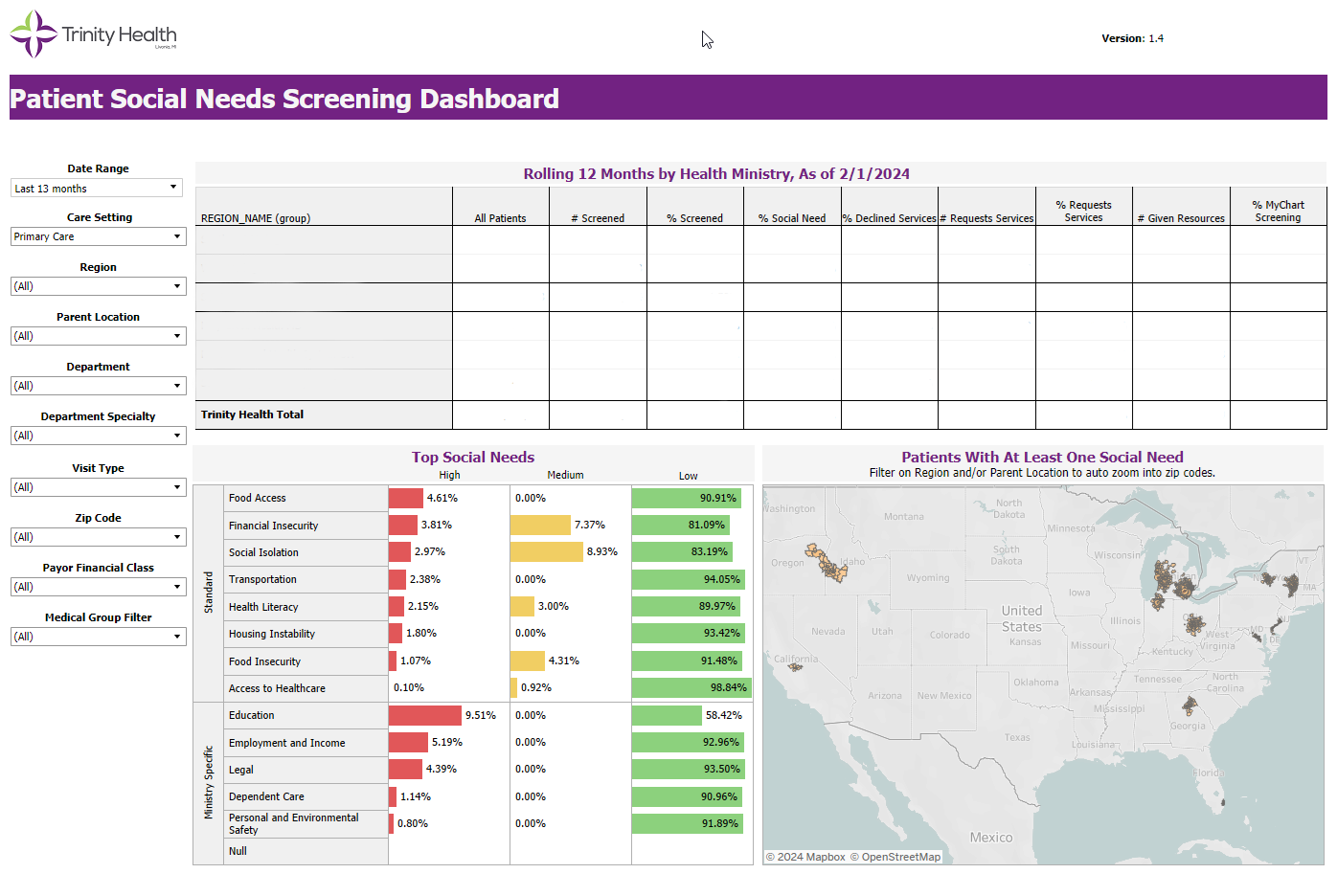
Also, our analytics team built a dashboard where we can easily pull social needs reports and segment our data by race, ethnicity, gender, and age. This is important because it allows us to better understand our patients’ highest needs and helps us focus our efforts on engaging the most appropriate community-based organizations to meet the needs of our patients.
The success of this tool is possible because of the integration between our social care and clinical care teams. Our community health workers document directly into the EHR, and our nurses and other providers can see that information immediately.
Q: What’s the biggest challenge with collecting social needs data?
Suleiman: Asking social needs related questions can be triggering for some patients. This information is extremely private, especially for patients who are vulnerable. And, depending on the patient’s trust of the provider, patients can be uncertain about how this information will be used.
Q: How do you handle that?
Suleiman: We’re currently implementing a national public health campaign called “why we ask” to effectively communicate the importance of collecting patient data related to social needs and key demographic information to advance health equity. We are working across our system interviewing colleagues who collect data and with patients and community members to understand their concerns about sharing this information. The goal is to enhance our process and better educate people on why we ask.
One of our core values is to “honor the sacredness and dignity of every person.” We do this by meeting our patients where they are and making it easy for them to get the services they need to live their best life. It is important that we are transparent about the role our health system plays in addressing social needs.
If we fall short of meeting our patients where they are — and if there are barriers for them to live their best life — then we need to acknowledge that and find solutions together. By listening to those being interviewed, we can create better strategies to address their concerns and help bridge the gap between social needs and health outcomes.
Q: Are there any other challenges?
Suleiman: In calendar year 2023, Trinity Health screened nearly 800,000 patients in primary care settings with more than 28 percent screening positive for at least one social need. However, only 9 percent of these patients request or accept help. While we would like the percentage of patients requesting help to increase, we understand that trust takes time. By earning that trust over time, hopefully we can see these numbers increase.
Q: Why do you think so few people ask for help?
Suleiman: Asking for help with basic needs puts people in a vulnerable position. It adds visibility to things people lack. There’s also the issue of trust that I mentioned earlier, and patients might not be fully confident that we can help them. It is important for all health systems to keep patients at the center of all we do and be transparent about our role and how this information will be used.
Spurlin: People may also not understand the ways in which healthcare providers can help. In some cultures, people are used to turning to their own families and communities for help only. Within Trinity Health, social care colleagues — especially community health workers — are part of and represent the communities as trusted partners who understand the needs of those we serve. These workers engage providers, patients, and community members. They also bridge the gaps between providers and patients/community members to give those we serve a path to resources.
Q: How do you fund the campaign to raise awareness of the importance of SIOH data?
Spurlin: We received a $12.5 million grant from the Centers for Disease Control and Prevention (CDC) that began in June 2023 to improve health equity for diabetes prevention. The grant, which focuses on the CDC’s National Diabetes Prevention Program, enabled us to create a network of partners (including diabetes prevention providers, community health workers, payers, clinicians, community-based organizations, professional organizations, and technology partners across a 16-state service area) to help adults over 65 and Black and Latinx/Hispanic adults 18 or older who are at risk for Type 2 diabetes. The “why we ask” education campaign is funded through this grant as well.
Q: What are your goals for 2024?
Spurlin: We plan on screening 100 percent of patients who attend the Diabetes Prevention Program at the beginning and at the end of our programing to ensure patients receive the help they need.
Suleiman: We’re also trying to help our medical practices refine the follow-up workflows for addressing social needs and create better reporting to enable us to make better associations between addressing social needs and health outcomes. Staff are doing the work, but they don’t yet capture it in a way that allows us to track information and tell a much larger story.
Lisa A. Eramo, MA, is a freelance healthcare writer based in Cranston, RI.