Nearly eight in 10 healthcare organizations currently collect social determinants of health (SDOH) data. However, challenges persist in leveraging this data to improve outcomes, a recent AHIMA survey found.
The Cleveland, OH-based MetroHealth Population Health Innovation Institute created the Institute of H.O.P.E. to address SDOH using evidence-based strategies. The acronym H.O.P.E. stands for Health, Opportunity, Partnership, and Empowerment as the institute’s goal is to help people live their healthiest lives.
The institute partners with numerous community-based organizations (CBOs), hospital associations, and healthcare systems to help patients get the services they need. AHIMA spoke with Susan M. Fuehrer, MBA, president of the Institute for H.O.P.E. about how her organization collects and uses SDOH data to benefit patients.
Q: What role do ICD-10-CM Z codes play in the work you do?
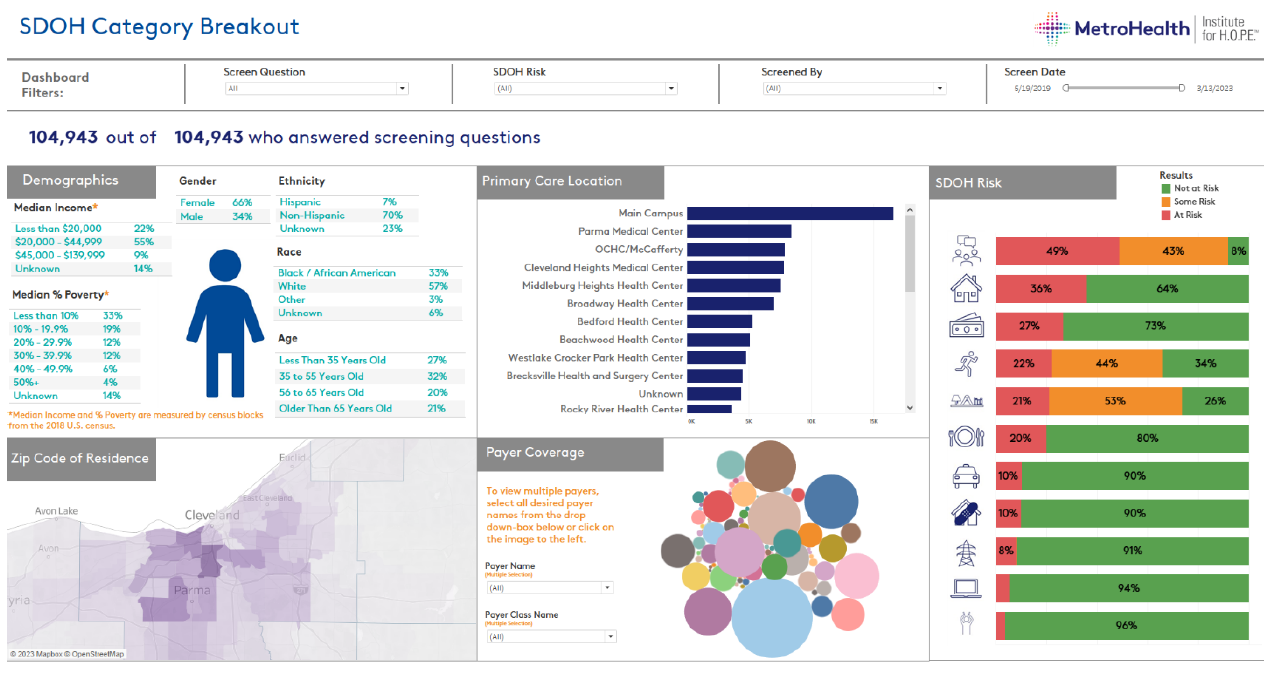
 A: Z codes are critical. We map patient screening responses to 18 different Z codes in 10 different SDOH domains (i.e., social isolation, stress, physical activity, transportation, food insecurity, housing stability, financial resource strain, intimate partner violence, housing problems, and utilities). The social drivers, documented via Z codes, can then be reviewed and addressed, in concert with the patient. In addition, given CMS [Centers for Medicare and Medicaid Services] regulations that require hospitals to screen all inpatients for five social drivers, this documentation helps us track our patients’ needs as well as how our clinical teams address those needs. We also screen for digital connectivity for which there is no Z code. However, we believe digital connectivity is an important social driver in today’s world.
A: Z codes are critical. We map patient screening responses to 18 different Z codes in 10 different SDOH domains (i.e., social isolation, stress, physical activity, transportation, food insecurity, housing stability, financial resource strain, intimate partner violence, housing problems, and utilities). The social drivers, documented via Z codes, can then be reviewed and addressed, in concert with the patient. In addition, given CMS [Centers for Medicare and Medicaid Services] regulations that require hospitals to screen all inpatients for five social drivers, this documentation helps us track our patients’ needs as well as how our clinical teams address those needs. We also screen for digital connectivity for which there is no Z code. However, we believe digital connectivity is an important social driver in today’s world.
SDOH screenings primarily occur through the portal, in person in the clinic, or via paper mail. Community health workers and care coordinators also help obtain the information. We also host events. For example, we held a minority men’s health fair, and if someone preregistered for the event and then completed the SDOH screening, we gave them a $15 gift card. We justified the cost by saving $15 in administrative fees. In addition, we’re moving toward screening all our inpatients as required by the CMS and The Joint Commission. Since July 2019, we have screened more than 100,00 patients and captured more than 60,000 Z codes.
Q: What is the biggest challenge in terms of leveraging Z codes?
A: Once you have the data, you have an obligation to do something about it. However, without a plan in place for referrals, clinicians are in a very tough spot. That’s why MetroHealth invested in an electronic referral platform. To date, nearly 300 organizations use this same platform. Healthcare organizations pay to use it, but it’s free to any 501(c)(3) CBO. All organizations that use it can communicate with each other. It’s about moving connections upstream and creating a synergy that doesn’t need to be healthcare system driven.
Q: What role can health information (HI) professionals play in helping organizations leverage SDOH data more effectively?
A: HI professionals help ensure accurate and consistent data collection that enables us to pair SDOH data with clinical outcomes. Without this information, we can’t do our work in a standardized, evidence-based way to show that addressing social determinants upstream helps us see reductions in unnecessary emergency department visits and admissions as well as a shorter length of stay. Of course, we also want to see improved health outcomes. However, that takes a bit longer. The data help us build a narrative for why addressing social determinants is so important with the ultimate goal of creating policy change to keep people healthy from the onset rather than wait until they are ill.
HI professionals can also help identify other ways to address social determinants. For example, our electronic health record includes an algorithm that automatically pings our trauma recovery team when someone screens positive for intimate partner violence. We’re also able to send education materials through our patient portal when someone screens positive for stress, physical inactivity, or social isolation.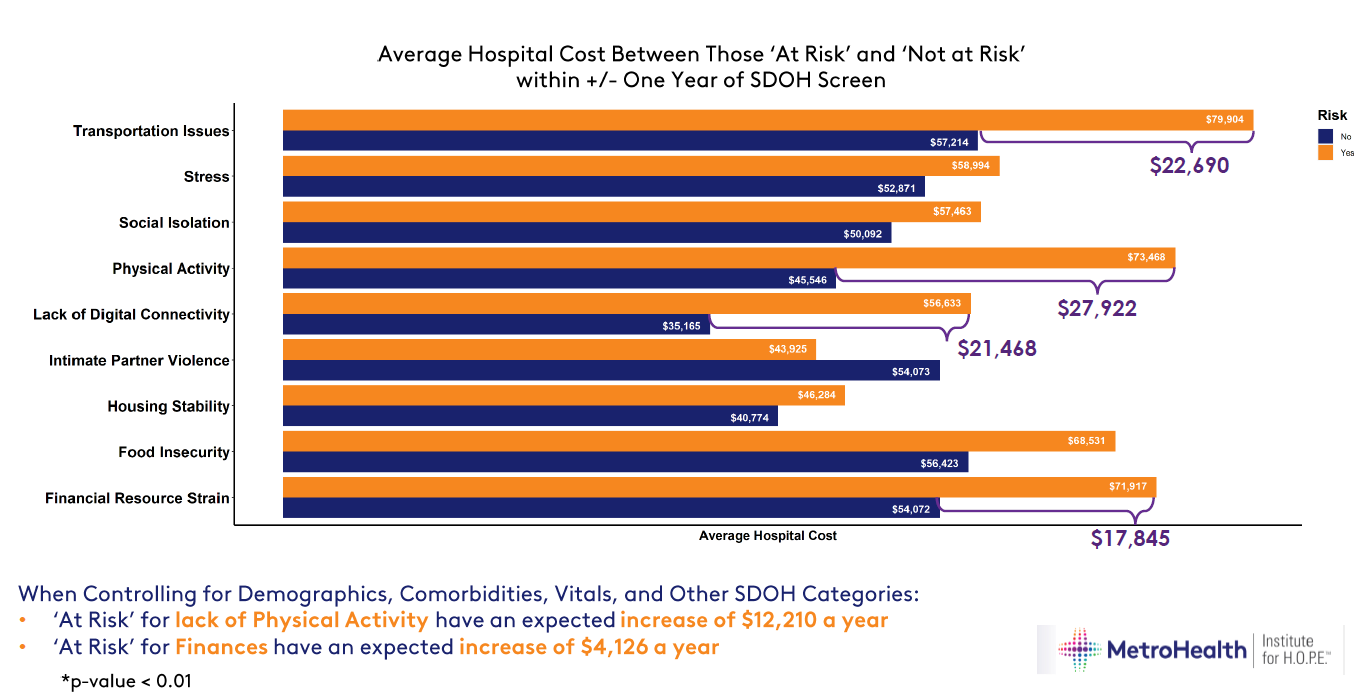
Q: How does the Institute for H.O.P.E. use SDOH data specifically?
A: The Z codes don’t automatically trigger a referral to a CBO, but they alert providers and staff that a referral may be appropriate and to obtain patient consent to participate in the referral platform. We also use SDOH data for contract negotiations, grants, philanthropic support, and to influence national policy reform. For example, we got a $900,000 grant from the Federal Communications Commission to address digital connectivity, and we’ve connected 1,000 homes in Cleveland to provide affordable internet to households. Our goal over time is to determine whether social interventions lead to a decrease in no shows, a decrease in inappropriate emergency department utilization, and a faster turnaround time for discharges.
Q: What has your data already shown?
A: We developed a dashboard internally that helps us monitor and filter the data in real time and intervene as early as possible. We’re also able to see the big picture. For example, we’ve been able to determine that those with food insecurity are 25 percent more likely to have three or more ED visits within the last year. They’re also 62 percent more likely to have 10 or more ED visits within the last year. We’ve also been able to show how unaddressed social determinants affect costs. For example, those at risk of physical activity have an expected increase of $12,210 a year. Those at risk for financial resource strain have an expected increase of $4,126 a year.
Q: What is your call to action for every HI professional?
A: Advocate for the collection of SDOH data. Then help your organization leverage it. Healthcare organizations can’t continue to spend more on helping people get healthy when we could use those same dollars earlier in the continuum.
Lisa A. Eramo, MA, is a freelance healthcare writer based in Cranston, RI.